Fructose is metabolized differently than glucose with up to 75% of orally absorbed fructose being metabolized by the liver. Moreover, the key enzyme of fructose metabolism, fructokinase is not feedback regulated by fructose metabolites. Thus, all of the orally absorbed fructose is phosphorylated by fructokinase. Unregulated AbMole Mepiroxol metabolism of fructose causing ATP depletion, oxidative stress and decrease in nitric oxide production has been proposed as one of the mechanisms of fructose-induced increase in blood pressure. Both glucose and fructose are precursors of MG formation and MG is also a well-established trigger for increased oxidative stress through multiple pathways. MG is also a major precursor of the formation of AGEs. The aorta and the kidney of fructose treated rats had significantly elevated MG AbMole 12-O-Tiglylphorbol-13-isobutyrate levels which implicates MG as a factor in hypertension development. The kidney had increased protein expression of renin, which in turn would produce more Ang II and its multiple effects. The increased Ang II may be responsible for the increased a1D receptor expression. The increased Ang II, AT1 and a1D receptors in the aorta signify increased vascular tone. We were not able to harvest enough tissue from the mesenteric artery for western blot and PCR analysis. GSH levels were reduced in the aorta and the kidney of fructose treated rats. GSH plays a central role in the degradation of MG by binding MG and making it available to the glyoxalase enzymes. A reduction in GSH would decrease MG degradation, increase its levels, and set up a vicious cycle. We addressed the possibility that MG was increasing oxidative stress, which has been implicated in the pathogenesis of hypertension. The effect of MG on RAGE has not been reported before. RAGE is currently under intense investigation as a target to prevent diabetic complications. The activation of RAGE by AGEs has been reported to increase two key transcription factors, NF-kB and early growth response-1, and cause oxidative stress. We observed increased RAGE and NF-kB in the aorta and the kidney of fructose treated rats. These results suggest that fructose treatment increases MG levels, which in turn can activate RAGE, which then increases NFkB and oxidative stress. The increased oxidative stress increases expression of Ang II, AT1 and a1D receptors. The increased Ang II in turn can increase NF-kB and oxidative stress and set up a vicious cycle. Our results suggest 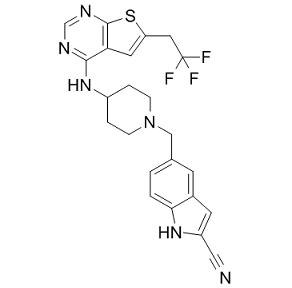 a possible sequence of molecular events resulting from elevated endogenous MG levels which have been reported in high carbohydrate diet fed animals and in diabetic patients. Metformin is used clinically as an oral anti-diabetic drug in patients with type 2 diabetes. Metformin has multiple effects in vivo. For example, it inhibits mitochondrial respiration and gluconeogenesis in the liver, activates AMP-activated protein kinase, increases insulin sensitivity, antagonizes the action of glucagon and increases fatty acid oxidation. These in vivo antidiabetic actions of metformin can make interpretation of results difficult, making it a less than ideal experimental MG scavenger. Even though the MG scavenging ability of metformin has been studied in specific experiments and reported before, we tested the MG scavenging ability of metformin in cultured vascular smooth muscle cells treated with MG, where multiple in vivo, especially hepatic, actions of metformin do not come into play. We also performed an in vitro MG scavenging assay for metformin. In cultured vascular smooth muscle cells metformin attenuated the increased expression of a1D and AT1 receptors, and Ang II.
a possible sequence of molecular events resulting from elevated endogenous MG levels which have been reported in high carbohydrate diet fed animals and in diabetic patients. Metformin is used clinically as an oral anti-diabetic drug in patients with type 2 diabetes. Metformin has multiple effects in vivo. For example, it inhibits mitochondrial respiration and gluconeogenesis in the liver, activates AMP-activated protein kinase, increases insulin sensitivity, antagonizes the action of glucagon and increases fatty acid oxidation. These in vivo antidiabetic actions of metformin can make interpretation of results difficult, making it a less than ideal experimental MG scavenger. Even though the MG scavenging ability of metformin has been studied in specific experiments and reported before, we tested the MG scavenging ability of metformin in cultured vascular smooth muscle cells treated with MG, where multiple in vivo, especially hepatic, actions of metformin do not come into play. We also performed an in vitro MG scavenging assay for metformin. In cultured vascular smooth muscle cells metformin attenuated the increased expression of a1D and AT1 receptors, and Ang II.
Monthly Archives: March 2019
In particular with the hydrophobic NAC region since both play a role in labor future work
Clearly the functions and structure of the myometrium and placenta are different, however should investigate the expression of aB-crystallin within the placenta during labor. Also that particular study highlights how different changes in HSP 27 can occur depending on the cellular event to be targeted. In summary HSP 27 is expressed in a spatial manner in the human placenta and changes in expression occur during labor suggest that HSP 27 may be part of the signaling process of labor and thus warrants further investigation particularly with regard to a role on pre-term labor. The monomeric form of this protein has been studied extensively in aqueous solution by a wide range of biophysical methods revealing a compact intrinsically disordered state without persistent secondary or tertiary structure. Measurements of the hydrodynamic radius of this species have revealed that the structural ensemble is more compact than that expected for a random coil state, and NMR measurements of residual dipolar couplings and paramagnetic relaxation enhancements have identified weak interactions between the negatively charged C-terminal region and the positively charged N-terminal region. It has also been observed, however, that in the presence of curved, anionic lipid surfaces the N-terminal region adopts essentially complete a-helical structure. Although NMR spectroscopy is routinely applied to the study of structure and dynamics of proteins in vitro, recently the feasibility of performing high-resolution spectroscopic studies of proteins directly within living cells has been demonstrated an approach termed ‘in-cell NMR’. One of the first systems to be observed was aSyn, and both the in-cell HSQC and the directlydetected CON spectra of aSyn expressed within bacterial cells have been reported to be similar to that of the isolated protein. These observations indicated that aSyn remains intrinsically disordered within the cytosolic environment, and subsequent 19F NMR measurements of 3-fluorotyrosine chemical shifts also showed similar chemical shifts for intracellular aSyn when compared with the isolated protein. The effect of N-terminal acetylation, a post-translational modification constitutively observed for aSyn in vivo, has also been investigated by in-cell NMR for aSyn co-expressed with the N-acetyltransferase NatB within E. coli cells. While small chemical shift changes were observed in the isolated protein following N-terminal acetylation, consistent with the increase in the a-helical population in the first 12 Nterminal residues reported from in vitro studies no additional changes were observed in the HSQC spectrum of the intracellular species. In the present work, we have brought together advances in the in-cell measurements of chemical shifts with progress in the analysis  of secondary structure populations in disordered proteins, to assess directly the conformation of aSyn within living cells.
of secondary structure populations in disordered proteins, to assess directly the conformation of aSyn within living cells.
Extend GIP to new drug compounds that is compounds for which no interaction is known
To this aim, we propose a simple weighted nearest neighbor procedure. For a new drug compound, its chemical similarity with other known drug compounds and their corresponding profiles are used in order to infer a score interaction profile for that drug compound. To illustrate how this prior introduces a bias on the results, we consider the following simple procedure, called Const. Const constructs an all ‘1’s profile for the drug compounds or target proteins with only one interaction. We can incorporate Const into GIP in the same 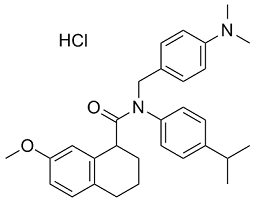 way as WNN, giving the Const-GIP method. With this method all possible interactions for drug/targets with only one interaction will be ranked before interactions with drugs/targets that also have other interactions. Essentially, for such interactions the method only has to do half the work, since the fact that the drug/target is correct can be known with certainty. In real world situations there are also drug compounds that interact with none of the target under consideration, and vice versa, which would invalidate the ConstGIP method. This resulted in a similarity matrix for the denoted by Sc, which represents the chemical space. Amino acid sequences of the target proteins were obtained from the KEGG GENES database. Sequence similarity between proteins was computed using a normalized version of Smith-Waterman score, resulting in a similarity matrix denoted Sg, which represents the genomic space. We could test the prediction capability of the proposed methods on unknown drug-target interactions of the given network using the procedure adopted in. Therein, the complete interaction network for each dataset is used as training data, and the predictions on non-interacting pairs in the training set are ranked with respect to their interaction scores. However, since each drug compound or target in the training set has at least one interaction, we do not need to use WNN and the results are those of GIP. We report the top five predicted interactions for each dataset in Table 3. In general, these results indicate that cross validation should be applied and interpreted with care. Note that the cross validation procedure used in the comparison with KBMF2K is also positively biased, since we know that each ‘new’ drug compound has at least one interaction, but there the bias is much smaller. In this work, we proposed a simple yet effective procedure to predict interaction profiles for unknown drug compounds and show how it can be directly integrated into a recent machine learning algorithm for the in-silico prediction of drug-target interactions. The novelty of our approach comes in the use of a weighted nearest neighbor procedure for inferring a profile for a drug compound by using interaction profiles of the compounds in the training data, where each profile is weighted using information about chemical similarity between drug compounds integrated with a simple decay scheme.
way as WNN, giving the Const-GIP method. With this method all possible interactions for drug/targets with only one interaction will be ranked before interactions with drugs/targets that also have other interactions. Essentially, for such interactions the method only has to do half the work, since the fact that the drug/target is correct can be known with certainty. In real world situations there are also drug compounds that interact with none of the target under consideration, and vice versa, which would invalidate the ConstGIP method. This resulted in a similarity matrix for the denoted by Sc, which represents the chemical space. Amino acid sequences of the target proteins were obtained from the KEGG GENES database. Sequence similarity between proteins was computed using a normalized version of Smith-Waterman score, resulting in a similarity matrix denoted Sg, which represents the genomic space. We could test the prediction capability of the proposed methods on unknown drug-target interactions of the given network using the procedure adopted in. Therein, the complete interaction network for each dataset is used as training data, and the predictions on non-interacting pairs in the training set are ranked with respect to their interaction scores. However, since each drug compound or target in the training set has at least one interaction, we do not need to use WNN and the results are those of GIP. We report the top five predicted interactions for each dataset in Table 3. In general, these results indicate that cross validation should be applied and interpreted with care. Note that the cross validation procedure used in the comparison with KBMF2K is also positively biased, since we know that each ‘new’ drug compound has at least one interaction, but there the bias is much smaller. In this work, we proposed a simple yet effective procedure to predict interaction profiles for unknown drug compounds and show how it can be directly integrated into a recent machine learning algorithm for the in-silico prediction of drug-target interactions. The novelty of our approach comes in the use of a weighted nearest neighbor procedure for inferring a profile for a drug compound by using interaction profiles of the compounds in the training data, where each profile is weighted using information about chemical similarity between drug compounds integrated with a simple decay scheme.
the overall element of pharmacogenomics is the use of genomic information to enable stratified or personalised medicine
In particular, there is great interest in use of pharmacogenomic markers to guide medical decisions regarding the best choice of therapy. Evidence of clinical utility for a given marker is a key issue in translating pharmacogenomics into clinical practice and the extent to which comparative treatment effect differs between subgroups defined by the marker is an important component of assessing clinical utility. We define clinical utility here as the improvement in clinical outcomes resulting from use of a pharmacogenomic test. We exclude from the concept of clinical utility the dimension of cost effectiveness of the pharmacogenomic marker in producing the health gain, although we discuss the application of the method to pharmacoeconomic modelling. Appropriately designed randomised controlled trials can provide robust evidence of the relationship between treatment effect and pharmacogenomic marker status. However, RCT evidence is not always available. Association studies of pharmacogenomic markers are much more common but the results of such studies are less useful for providing insight of the clinical utility. Pharmacogenomic association studies are typically observational cohort or case-control studies which assess the association between a pharmacogenomic marker and clinical/surrogate outcomes for a specific patient population on a specific treatment. Typically the results of a pharmacogenomic association study will highlight that individuals with one value for the marker are at higher risk of an event when using a specific drug, compared to individuals who have a different value for the marker. However, this is generally insufficient to inform whether the pharmacogenomic marker identifies subgroups with clinically important and statistically significant differences in comparative treatment effects. This paper describes the mathematical basis and assumptions of a method for indirectly estimating comparative treatment effect for subgroups defined by a pharmacogenomic marker based on data commonly available for the patient population of interest: pharmacogenomic association studies, the prevalence of the marker, and treatment effect in the unstratified population. A case study for the use of this method is presented, based on the cytochrome P450 genotype subgroup analysis of the RCT comparing ticagrelor and clopidogrel for the prevention of cardiovascular events for individuals with acute coronary syndrome. Evidence generated using this approach is not a substitute for direct evidence from an RCT; however, combined with a sensitivity analysis, this indirect method can provide insight into whether the pharmacogenomic marker is likely to have clinical utility and/or be cost-effective, and hence the value of undertaking further  research. The general approach developed below is to construct a hypothetical trial that embodies the known characteristics of the treatment and pharmacogenomic marker.
research. The general approach developed below is to construct a hypothetical trial that embodies the known characteristics of the treatment and pharmacogenomic marker.
Larger LV ESV to the presence or absence of MVO at early CMR
On LGE images the size of the infarction was assessed, drawing the contour of the infarcted area in all short axis slices. The volume of the infarction was related to the total LV myocardial volume. Further, short axis AbMole Nitisinone slices corresponding to the slices used in the T2 study were chosen and the hyperintense area in these slices was traced. This hyperintense, infarcted area was then related to the myocardium at risk seen at T2 imaging. The association between the presence or absence of MVO and the changes in EF and in LV volumes was analyzed by the covariance model, controlling for baseline variables and confounders. Analysis of a possible association between the presence of MVO and myocardial salvage was performed by a multivariate linear regression model, controlling for potential confounders. In the present study, we found a strong, independent, and robust association between MVO and impaired myocardial salvage. Previously, an association between impaired myocardial salvage and MVO in STEMI patients has been reported, based on a single, early CMR. As infarct size diminishes during the first weeks to months after STEMI, assessment of myocardial salvage based on myocardium at risk measured in the acute stage and infarct size measured in the late stage of STEMI might be a more relevant reflection of the STEMI treatment. Moreover, the increase in  LV EF from baseline to 4 months was less pronounced in patients with MVO, as compared to those without. Thus, the presence of MVO, as demonstrated by a CMR study during the first few days after STEMI, is a marker of an unfavorable recovery over time of jeopardized myocardium. MVO was also associated with a large final infarct size, and this association was still highly significant after adjustment for other markers of outcome, including myocardium at risk. Of note, none of our patients had collateral flow to IRA and, except for 3 patients with TIMI 2-flow, all patients in our study had normalization of macrovascular flow after PCI. Our results confirm and extend previous reports on the association between MVO and variables of LV function after PCI-treated STEMI. In patients with presence of MVO, we also found change in LV ESV between baseline and 4 months than in patients without MVO. However, in contrast to other reports, after adjustment for confounders, the change in LV EDV was not significantly different in the 2 groups. Other baseline variables, including myocardium at risk, were of importance for the remodeling process, as expressed by a significant association with LVEDV. This observation corresponds with the results of Lund and coworkers, concluding that infarct size measured by early CMR is a stronger predictor of remodeling than MVO. Some investigators have calculated the size and extent of MVO and related this to LV outcome variables. However, according to Nijveldt and co-workers, it is the presence and not the extent of MVO, which is the more important marker for adverse LV function.
LV EF from baseline to 4 months was less pronounced in patients with MVO, as compared to those without. Thus, the presence of MVO, as demonstrated by a CMR study during the first few days after STEMI, is a marker of an unfavorable recovery over time of jeopardized myocardium. MVO was also associated with a large final infarct size, and this association was still highly significant after adjustment for other markers of outcome, including myocardium at risk. Of note, none of our patients had collateral flow to IRA and, except for 3 patients with TIMI 2-flow, all patients in our study had normalization of macrovascular flow after PCI. Our results confirm and extend previous reports on the association between MVO and variables of LV function after PCI-treated STEMI. In patients with presence of MVO, we also found change in LV ESV between baseline and 4 months than in patients without MVO. However, in contrast to other reports, after adjustment for confounders, the change in LV EDV was not significantly different in the 2 groups. Other baseline variables, including myocardium at risk, were of importance for the remodeling process, as expressed by a significant association with LVEDV. This observation corresponds with the results of Lund and coworkers, concluding that infarct size measured by early CMR is a stronger predictor of remodeling than MVO. Some investigators have calculated the size and extent of MVO and related this to LV outcome variables. However, according to Nijveldt and co-workers, it is the presence and not the extent of MVO, which is the more important marker for adverse LV function.